Allergy testing and desensitization. How do we test for allergies?
An allergic reaction represents an immune system response to a substance (an allergen) that it perceives as dangerous. The scope of potential allergens is essentially limitless and encompasses virtually anything that can be eaten, inhaled or touched. Common allergens include pollen, foods, dust, moulds, venoms, fur and medications.
Symptoms of allergic reaction range from mild to severe to life-threatening. They can include sneezing; itching or prickling sensations; localized swelling or rash; hives; flushing; or throbbing in ears. Seek immediate care if you develop symptoms of a severe allergic reaction such as sudden and severe hives; swelling around the mouth or eyes, or generalized swelling; palpitations; immediate feeling of agitation or unease; swelling in mouth and throat; difficulty breathing; or convulsions.
What you can do
One of the easiest and most inexpensive ways of identifying allergies is to keep a log of your symptoms and any pertinent details: when symptoms occur (including which seasons), possible causes (the house has just been cleaned, you’ve been in contact with some type of chemical, symptoms began after you drank milk, etc.), and when symptoms get worse or better. Over time, significant patterns may become evident.
If you have a mild reaction to a food, try eliminating it from your diet and watch for changes in your symptoms. Or, if you suspect an allergy to a substance at work, watch how you feel while you are on vacation or away for a while. Do your symptoms decline?
The most effective way to treat an allergy is to avoid exposure to the offending substance. This is particularly true of food allergies, which can get worse with each exposure.
Call your doctor if your symptoms are severe or significantly interfere with your daily activities. In many cases, the sufferer knows exactly what they are allergic to. In other cases, careful questioning by a doctor will help narrow the list and possibly pinpoint the allergen. A person’s entire lifestyle and history must be considered, including past medical history, allergies among close relatives, hobbies, food reactions, emotional health and work environment. Allergy testing is reserved for cases in which this kind of intense questioning fails to identify the cause(s).
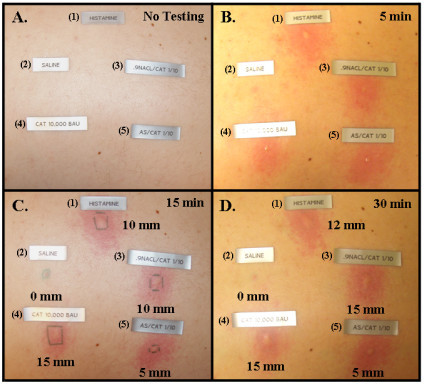
If the above questioning fails to identify a cause for your allergy, your doctor or allergy specialist (allergist) will probably use provocation testing to identify the offending substances. An example is skin testing, which is inexpensive, relatively convenient, and can be very useful for identifying respiratory allergies (dust mites, animal dander, pollens, etc.) and allergies to insect bites and certain drugs such as penicillin. Skin testing may not be appropriate for food allergies.
These tests, in which a tiny amount of the allergen is injected just under the skin’s surface, demand skill and caution. The tester should know what kind of reactions you have had in the past. Stay in the testing centre for at least 20 minutes after the allergen is applied, and do not take any antihistamine drugs before these tests.
Allergies to inhaled substances can be identified by using RAST (radioallergosorbent) or ELISA (enzyme-linked immunosorbent assay) tests. The great advantage of these blood tests is they pose no risk of provoking a system-wide reaction.
Food allergies may be diagnosed by using a double-blind test. Suspected foods and innocuous substances (placebo) are coded and administered by doing it in this way neither the patient nor the tester knows which is being given. The identity of the substances is revealed only after a potential reaction has occurred.
Other tests proclaimed in the media, such as cytotoxic testing, neutralization, yeast testing or other tests not mentioned here can be dangerous. Their scientific integrity is largely unproven.
Treatment of allergies
Desensitization (hyposensitization) treatment may be appropriate if you are suffering from allergic asthma or severe allergic rhinitis (runny nose) that persists despite avoidance and medications. This treatment is based on the theory that a person will become less sensitive to a substance when they are repeatedly exposed to it. Therapy involves injection with a minute amount of the offending allergen suspended in a liquid solution, followed by weekly or twice-weekly injections of increasingly larger concentrations of allergen. This process is continued until the person can tolerate exposure to a certain amount of allergen with no or only mild symptoms. This maintenance dose is then injected every two to four weeks for several years.
Results with desensitization are mixed. Some people with hay fever become more tolerant of natural pollen over subsequent seasons while on therapy, some people stop having symptoms altogether, and some people show no improvement at all.
If you and your doctor decide that desensitization treatment is appropriate, remember that treatment should be sought before allergy season begins, and should be cut back during peak season. If you are travelling, talk to your doctor about the possibility of taking your maintenance dose with you, to have injected while you are away.
Hay Fever (Allergy)
Hay fever is an allergic reaction to windborne pollens and fungal spores. The moment a pollen or spore lands on the moist lining of the eye, the nose or the lung airways, the allergen is released and if the person is allergic to the pollen or spores, a reaction occurs at once by sneezing, in an attempt to get rid of it. It is extremely common and can appear or disappear at any stage of life. Allergies left untreated can cause sinus swelling leading to chronic sinusitis.
The trigger allergens start with tree pollens (acacia, cypress, oak, olive and plane) in early spring (August), followed from September through to the end of February by the grass pollens (Bermuda, Eragrostis, Lolium and rye). Weed pollens (English, plantain and cosmos) occurs for a short period in late summer and fungal or mould spores (Alternaria, Cladosporium and Epicoccum) predominate in Autumn and Spring but tend to be less problematic than pollen. The seasonal mix varies in different parts of the country.
Hay fever symptoms may persist for weeks or months and reappear whenever the offending pollen or other allergen comes into season again — usually the same time every year. It’s impossible to predict who will develop hay fever, although it often appears in people who have other allergies, such as asthma and dermatitis, or it tends to run in families.
Note your symptoms
A hay fever sufferer may be allergic to one or more pollens. For reasons unknown, their antibodies react with the pollen, prompting the release of histamine. This causes the lining of the nose, sinuses, eyes and eyelids to become inflamed. These areas, as well as the roof of the mouth and the throat, start to itch either gradually or suddenly.
Other symptoms are tearing; swelling of the eyes, frequent and sometimes violent sneezing (as many as 10 to 20 sneezes in a row) and very clear, watery secretions from the nose. Some people develop headaches and insomnia, lose their appetite and are generally irritable and depressed. As the season progresses, coughing and asthmatic wheezing may be added to the symptom list. Episodes last for about 30 minutes and tend to occur several times a day. Despite the name, fever is not a symptom. Infants can develop hay fever symptoms in response to certain foods.

What you can do
In most cases, hay fever sufferers can accurately diagnose and effectively treat their own condition. The most effective way of controlling symptoms is to avoid the responsible allergen(s). Stay indoors when pollen counts are high, particularly on dry, windy days. And in addition try to keep your home and workplace allergen-free:
- Keep doors and windows shut
- Cover pillows and mattresses with plastic
- Replace animal products (such as wool and horsehair) with synthetic materials (such as foam mattress and pillows, and acrylics)
- Remove household fixtures prone to collecting dust (including drapes, carpets, and bedspreads)
Symptoms of mild hay fever may be relieved by non-prescription antihistamines and oral decongestants. Oral antihistamines block the action of inflammation-producing histamine. Their drying effect offers relief. The effectiveness of antihistamines varies among people, as do side effects such as drowsiness and dryness of the throat and mouth.
Try taking non-prescription decongestant tablets along with antihistamines to reduce drowsiness and runny nose. Long-term use of over-the-counter nasal sprays and eye drops should be avoided; they can be habit forming and may cause a “rebound effect,” making symptoms much worse. If you have a chronic illness, are pregnant, or routinely take prescribed or over-the-counter medications, talk to your doctor or pharmacist before taking any new medications.
Treatment options
In addition to asking numerous questions about lifestyle, a doctor will do a physical examination and possibly inspect samples of nasal secretions for high concentrations of certain white cells (eosinophils), which can indicate an allergic reaction. A doctor should also be able to help identify the offending pollens.
You may be asked to keep a diary of symptoms to help determine which allergens are responsible. For persistent problems, you may be referred to an allergist (a doctor specializing in allergies). Stronger antihistamines may be prescribed for severe cases. Newer preparations result in less sedation but tend to be more expensive and may have interaction with certain other medications. If prescribed, follow your doctor’s instructions carefully.
Should these fail, even stronger medications, such as corticosteroids, may be considered and can be given as a nasal spray. It is more effective in preventing than treating acute episodes. Several weeks of this relatively expensive therapy may be needed before improvement is noticed.
Corticosteroid nasal preparations, such as beclomethasone and fluticasone require a couple of weeks to be of benefit. Because of the side effects, oral corticosteroids are only prescribed in the severest cases.
Desensitization may be recommended if the response or tolerance to these medications is poor, oral corticosteroids are needed, or allergic asthma develops. Desensitization is expensive and involves long-term exposure to minute amounts of the offending allergen, and is effective in 70 per cent to 80 per cent of sufferers.
Important
Call your doctor if symptoms start to interfere significantly with your daily routine. A doctor will be able to confirm if you are suffering from hay fever rather than some other condition, such as a viral infection. In addition, call your doctor if your symptoms are not relieved with over-the-counter medications or if you suffer from hay fever and develop symptoms of an ear infection or a sinus infection (also called sinusitis). Symptoms of sinusitis include pain and swelling of the eyes or cheeks; fever; nasal discharge that has turned from clear to coloured; and ear pain or a feeling of fullness in the ear.
Kind Regards
Shawn Herbst
Media Liaison Officer
Netcare Limited
Netcare 911